HPV Vaccine prevents Cancer in Males as well as Females, Researchers Say
Researchers affirm the HPV vaccine's efficacy in preventing cancer across genders, offering crucial protection against HPV-related malignancies. Explore how this vaccine serves as a vital tool in safeguarding both males and females against the threat of cancer.
- A new analysis suggests the HPV vaccine may be more effective in males than in females.
- Many people believe HPV affects females specifically, but this is a misconception.
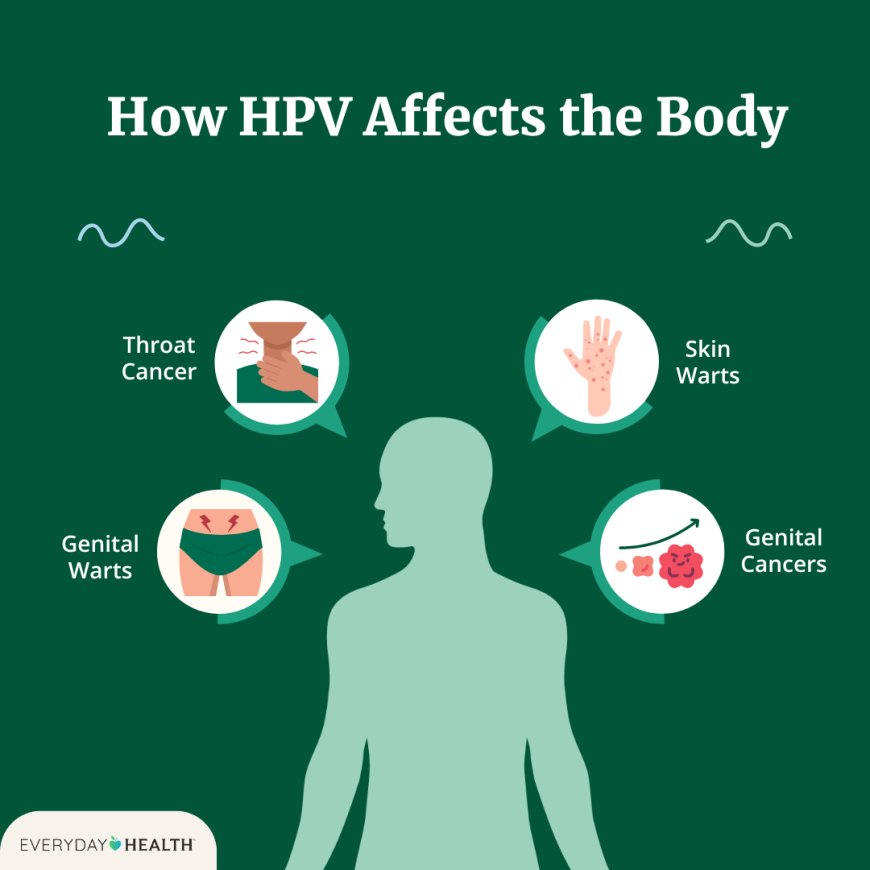
- HPV has been linked to throat, anal, and anal canal cancers in both sexes, as well as penis cancer in males and cervical, vaginal, and vulvar cancer in females.
- Misconceptions about HPV hold back vaccination rates in males and females, which experts believe should be higher.
Cervical cancer is the most common type of female cancer linked to the human papillomavirus or HPV.
Each year, almost 200,000 females are diagnosed with cervical pre-cancer, according to the Centers for Disease Control and Prevention (CDC)Trusted Source, and about 11,100 females are diagnosed with HPV-caused cervical cancer. Roughly 4,000 females in the United States die annually from the disease. HPV infections typically resolve within a year or two.
However, some types of HPV can lead to the development of cancer in both males and females, resulting in about 36,000 cases of cancer each year. In fact, almost everyone will get infected at some point in their lifetime by a strain of HPV, according to the CDCTrusted Source.
There is a vaccine for HPV that can prevent over 90%Trusted Source of HPV-related cancers. In 2022, however, just 38.6%Trusted Source of young people in the U.S. had received at least one of the two recommended doses. Despite the risks associated with HPV in either sex, girls are more likely to be vaccinated against it than boys.
Now, new research reveals that HPV vaccinations may reduce the risk of HPV-related cancers by as much as 56% in males and 36% in females.
The findings, which were presented at the annual meeting of the American Society of Clinical Oncology May 31–June 4 in Chicago, IL, have not been published in a peer-reviewed scientific journal.
Daniel Ganjian, MD, FAAP, board certified pediatrician at Providence Saint John’s Health Center in Santa Monica, CA, not involved in the research, explained to Medical News Today:
“The incidence of HPV-related cancers in men is significant. According to the CDCTrusted Source, about 4 out of every 10 cases of cancer caused by HPV occur among men, with over 15,000 men getting cancers caused by HPV every year in the U.S. The types of HPV that cause cancer can affect both women and men, with HPV-related throat cancers more often affecting men and rapidly increasing in the developed world.”
How effective is the HPV vaccine at preventing cancer?In females, the HPV virus is linked to the development of cervical, vaginal, and vulvar cancers. In males, HPV is associated with cancer of the penis. In both sexes, HPV can lead to throat cancer, as well as anal and anal canal cancer.
The HPV vaccine can prevent more than 90% of vaginal, cervical, and vulvar “pre-cancers,” involving abnormal cells that indicate a higher risk of cancer later on.
The authors of the new research compared about 1.7 million individuals who had been HPV-vaccinated with another similarly sized and age-matched group who had not been vaccinated.
The researchers found there were 3.4 cases of HPV-related cancer per 100,000 vaccinated males, while there were more than double that amount, 7.5 cases per the same number of unvaccinated males.
For females, the difference was also significant: There were 11.5 cases of HPV-related cancer per 100,000 vaccinated females, and 15.8 cases per 100,000 unvaccinated females.
Rachel Goldberg, LMFT, a therapist in Los Angeles, CA, not involved in the study, has counseled families about HPV vaccines.
“For decades, women have been told about the importance of Pap smears to catch any early signs,” she told MNT.
“Most women know of at least one person [who] had to go through a minor procedure to remove abnormal cells thought to be HPV-related. It’s often a woman in her 20s or 30s,” Goldberg said.
Goldberg reported a rise in male HPV cancers, particularly among men from 40 to 60 years of age.
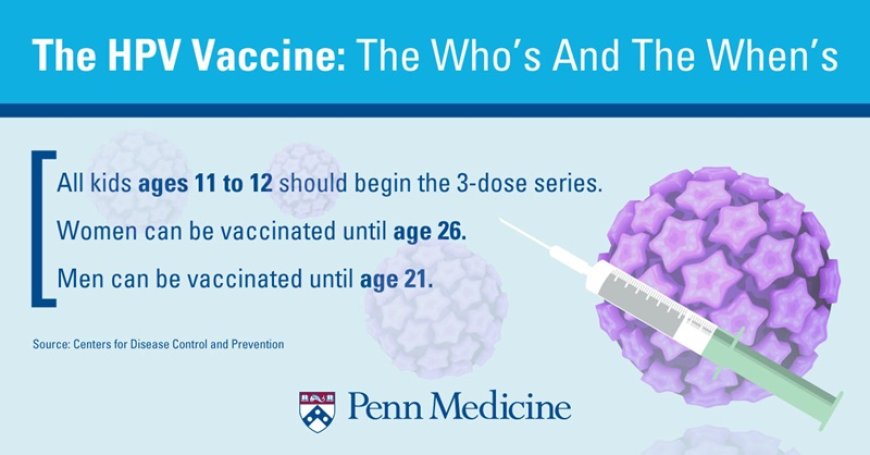
Why is it important to increase HPT vaccination in children?The CDC recommendsTrusted Source children receive two doses of HPV vaccine starting at ages 11 to 12, although the two inoculations can begin as early as nine years of age.
For children who do not receive their first HPV vaccination before they are 15, three inoculations, not two, are required for optimal protection.
“It’s important to note that HPV vaccination prevents new HPV infections but does not treat existing HPV infections or diseases. The vaccine works best when given before any exposure to HPV,” Ganjian said.
Goldberg noted that some parents may choose to delay vaccinating their children against HPV, perhaps because they are not yet sexually active.
“Over time, parents may believe it’s too late, their child ages out of being under their care, or they assume it won’t affect their child because of his [or her] level of responsibility, not understanding how easily HPV spreads,” Goldberg explained.
“The value of the HPV vaccine for males is known among physicians, but awareness and vaccine uptake among men have been low,” Ganjian said.
Other misconceptions may contribute to stigma around HPV for young males, Goldberg noted.
“It is still primarily viewed as a protective measure for girls, with some parents holding the belief that vaccinating their sons is only to protect their potential future female partners,” Goldberg
What's Your Reaction?